Melissa Foster, N.P., discusses how this lesser known cancer can go undetected – and what you and your provider can do about it.
According to the American Cancer Society, 1 in 78 women will develop ovarian cancer in their lifetime. As an oncology certified nurse practitioner, I am passionate about cancer prevention and a strong advocate of routine visits for women of all ages. These annual visits provide an opportunity to screen for and catch a lot of health issues before they become bigger problems. But with a lesser known cancer that can fly under the radar and disguise itself as other disorders or conditions, it takes being in tune with your body as well as a real team effort from you and your provider to get in front of it. From recognizing possible symptoms to knowing risk factors and methods of risk reduction, we’ll discuss how you and your doctor can work together against ovarian cancer.
Screening Shortcomings
While routine screening tests are used for detection of many other health issues when no symptoms are present, there are currently no effective screening techniques to detect ovarian cancer in pre-cancerous or early stages among the general population. One test that has been studied is the CA-125 blood test. Many women with ovarian cancer have high levels of CA-125 in their blood, and the CA-125 blood test can detect these high levels. However, not all women who have ovarian cancer have high levels of CA-125, and high CA-125 can indicate other conditions such as endometriosis and pelvic inflammatory disease. Frequent pelvic ultrasounds have also been used for screening. Unfortunately, each study of these screening tests has determined a high false positive rate and no decrease in the number of deaths from ovarian cancer-related causes.
Research is being done to come up with more accurate screening tests, but as of now it is not recommended that women with average risk of ovarian cancer get screened routinely. Since screening remains difficult, it is important to see your gynecologic provider on a regular basis (see annual exam blog reference) and communicate any symptoms you may have.
Understanding Female Pelvic Anatomy
Female anatomy is beautiful and complicated, and it can play a part in ovarian cancer going undetected. Ovaries are part of the female reproductive system, and they are tasked with two main jobs: storing and producing eggs and creating the female hormones that prompt ovulation and menstruation (estrogen and progesterone). The fallopian tubes on either side of the uterus transport an egg from the ovary to the uterus during ovulation. It is now thought that ovarian cancer may originate within the fallopian tubes.
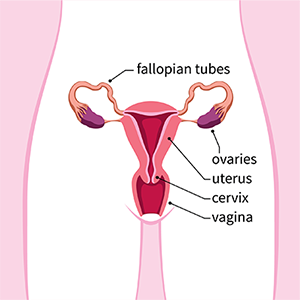

An important thing to realize about female anatomy is how medical graphics distort how everything really lies in your body. It can appear that the intestines are separate from your pelvic organs because medical graphics often show each in isolation from the other. However, if you compare the first graphic of the reproductive system with the second graphic of other organs, you can see how they overlap. That can make determining the cause of any symptoms you have very difficult.
What Are the Symptoms? (They Can Be Vague)
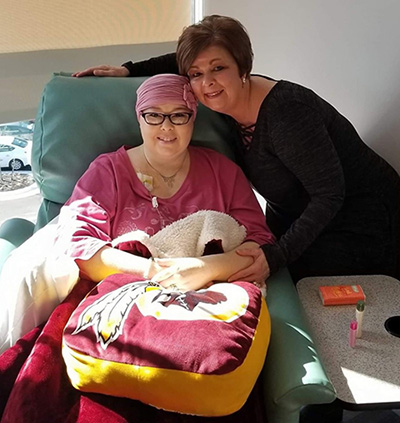
“Wendy suffered from Irritable Bowel Syndrome and dealt with bloating and discomfort for years, and we assumed her symptoms were related to IBS” says Judy Smith, a long-time VPFW call center employee, of her daughter Wendy. At age 44, Wendy went to see Dr. Stephen Pound to discuss dysfunctional uterine bleeding and bloating. “Since we have not yet found a reliable screening test for ovarian cancer, we have to keep a high index of suspicion,” says Dr. Pound. He ordered an ultrasound, and a mass was discovered in Wendy’s ovary. She was referred to an oncologist and diagnosed with ovarian cancer and uterine cancer. Fortunately, they appear to have caught it in time: with treatment, determination, and a true team effort between Wendy and her health care team, she has overcome both.
But Wendy’s cancer is an example of why the symptoms of ovarian cancer are often referred to as “vague.” They can be similar to bowel/gastrointestinal complaints. “The signs and symptoms are frequently downplayed by patients” says Dr. Pound. “It is important to report to your physician if you feel bloating, pelvic pain, difficulty eating, or difficulty finishing a meal.”
The most common symptoms to note include:
- Bloating
- Pelvic/abdominal pain
- Difficulty eating/feeling full
- Urinary frequency
- Change in bowel habits
When to See a Doctor
As you can see from the list of symptoms above, each one can often be explained away by another cause. Having any of these symptoms individually or together occasionally does not mean you have or are at increased risk for ovarian cancer. However, if one or more of these symptoms is happening several times a month and is a new onset, you should see your provider for an evaluation.
Evaluation for Ovarian Cancer: What to Expect
Evaluation for ovarian cancer will include a physical exam. Depending on the size, an ovarian mass can be felt on a bimanual exam (a pelvic exam where the provider uses two hands), even if there are no symptoms. This is another reason to maintain regular visits with your gynecologic provider. A transvaginal ultrasound will likely be performed as well. Blood levels may or may not be drawn, depending on the findings of the physical exam and ultrasound.
How can you help your provider?
Be prepared to answer a lot of questions about your bowel health and whether you are up to date with a colon cancer screening. As mentioned above, many symptoms can also be related to other causes including several gastrointestinal diagnoses. Be assured your provider is not trying to explain away your symptoms but trying to be your advocate in case an ovarian cancer is not found.
Risk Factors for Ovarian Cancer
There are several risk factors of ovarian cancer that you should be aware of and discuss with your provider. The following are risks factors for epithelial cancer of the ovaries, where cancer develops in the cells that cover the outer surface of the ovary. It’s the most common form of ovarian cancer, accounting for 85-90% of all cancers of the ovaries. They do not apply to other, less common types of ovarian cancer such as germ cell and stromal tumors.
Aging
Over half of all ovarian cancers are diagnosed after the age of 63. It is rarely detected in women under 40.
Obesity
There is no clear reason why obesity is an increased risk factor for ovarian cancer. We also know that women who are obese have higher mortality rates.
Older age at first pregnancy
Older age at first pregnancy (after age 35) or never carrying a term pregnancy is also an increased risk factor for women.
Post-Menopausal Hormone Therapy
Hormone therapy, an effective treatment for menopause, elevates the risk slightly compared to women who never use hormone therapy.
Family History and Genetic Mutations
Genetic mutations are abnormal alterations in genes that can be passed on from a mother or father to a child. Mutations in the BRCA genes (BReast CAncer genes) are rare in the general population – about 1 in 400 have one. The risk of developing ovarian cancer increases from 1 or 2% (among women generally) to 30-50% among those with BRCA1 mutations and 10-25% among those with BRCA2 mutations. Relative risk for those with a BRCA gene mutation increases with age, doubling between ages 40-50 for both BRCA 1 and 2.
Genetic mutations are also linked to Hereditary Nonpolyposis Colon Cancer (HNPCC), a type of bowel cancer predisposition. Another name for HNPCC is “Lynch Syndrome.” Women with certain genetic mutations in the Lynch Syndrome genes have a 10 to 17% chance of ovarian cancer as well as an increased risk of colon and uterine cancers.
Hereditary breast and ovarian cancer syndrome (HBOC) is present in 5% of women with breast cancer and 10% of those with ovarian cancer. You should discuss the possibility of HBOC with your provider if your personal or family history includes:
- Ovarian cancer
- Breast cancer diagnosed at age 50 or younger
- Two primary breast cancers, meaning they have occurred in the same individual or same side of the family
- Male breast cancer in a relative (of any degree)
- Triple negative breast cancer
- Pancreatic cancer with an additional HBCO- associated cancer (including breast, ovarian, and pancreatic cancer) in the same individual or on the same side of the family
- Ashkenazi Jewish ancestry with an HBOC-associated cancer (including breast, ovarian, and pancreatic cancer) in the same individual or on the same side of the family
- A previously identified BRCA mutation in the family
There are additional, more rare genetic disorders that can be linked to ovarian cancer that can be found on the American Cancer Society website. Talk to your provider if you would like to have genetic testing done to determine if you have a genetic mutation that would put you at a higher risk for ovarian cancer or breast cancer.
How to Reduce Your Risk
Through years of data and research, there are a few factors found to reduce the risk of ovarian cancer for some women:
- Permanent sterilization with tubal ligation (having your “tubes tied”)
- Complete removal of fallopian tubes (a preferred method of permanent sterilization by the Society of Gynecologic Oncologists)
- Removal of ovaries
- Childbearing
- Breastfeeding
- Use of oral contraceptive (“the pill”)
Know the Signs and Talk to Your Provider

As you can see, screening of ovarian cancer for the general population relies heavily on routine physical exams and discussion of any concerning symptoms with providers. As a caring mother, Judy Smith can attest to how stealthy the disease can be. “Cancer? My daughter has cancer? How could I let this happen? I worked for VPFW for 23 years. How did I not see the signs? Maybe because she had irritable bowel syndrome. Maybe because I thought this would not happen to her,” Judy conceded. “The signs of ovarian cancer can be so subtle. Know them, listen to your body, and see your gynecologist on an annual basis.”
Remember that if you are experiencing any health issues, large or small, your providers are here to listen and help you figure out what’s going on. Our number one goal is to help you feel better. We hope you take comfort in Judy’s favorite quote: “She stood in the storm and when the wind did not blow her way, she adjusted the sails.”
To make an appointment with an OB/GYN provider at one of our Richmond, VA, locations, call VPFW at 804-897-2100 or message us to schedule online.
