Nicole Kelleher, M.D., answers questions she wishes every woman would ask about mammograms and breast health.
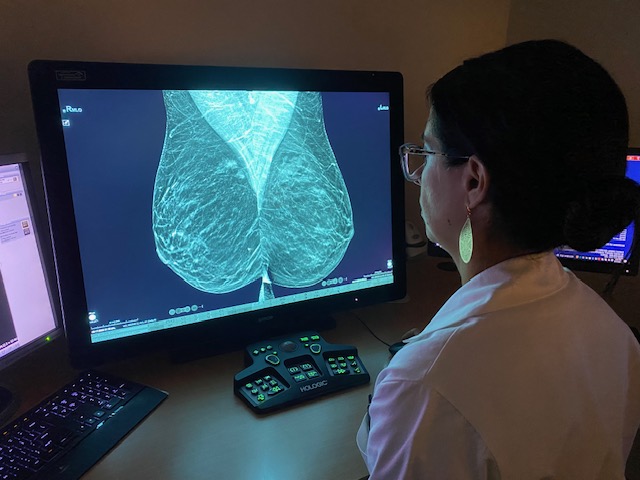
If you’ve ever had a mammogram at VPFW, there’s a good chance it was read by Dr. Nicole Kelleher. Dr. Kelleher reads mammograms as part of her job as a breast radiologist at Radiology Associates of Richmond. We were delighted to have the opportunity to interview this fellow advocate for annual screening mammograms and breast health to get a peek behind the curtain and learn what a radiologist wishes all women knew about mammography.
How did you become passionate about breast cancer detection?

Most of us have been affected by a breast cancer diagnosis in one way, shape, or form. After finishing college and while working on my Paramedic degree and Master’s in Anatomy, I worked in a Clinical Pharmacology lab at VCU. My main supervisor at VCU (who ended up being like a second mother to me, aka Mamma San) and her daughter were both breast cancer survivors and advocates of breast cancer screening. These women taught me about breast cancer and the importance of early detection through screening mammography, when chances of survival are greatest.
Having been diagnosed 30 and 10 years prior, respectively, both women know first-hand how critical early detection is in the fight against breast cancer. I have been passionate about working to diagnose breast cancer in its earliest stages ever since I first got to know these two remarkable women. Now, as a breast radiologist, it has become my mission in life to detect a patient’s breast cancer at its smallest detectable size.
What is the difference between a screening mammogram and a diagnostic mammogram?
A screening mammogram is done on a woman without any symptoms or concerns. Screening mammograms are a way for breast cancer to be detected in its earliest stages of development, before symptoms may be present.
A diagnostic mammogram is done on a woman who has noticed a change in her breast, such as a “lump” or thickening, focal and/or persistent pain, nipple changes, spontaneous nipple discharge, etc., or if the referring clinician has a concern on a patient’s clinical breast exam. While a screening mammogram usually takes about 15 minutes, a diagnostic mammogram may take a little longer if the tech needs to take more images and/or focus on a specific area of interest.
What is a radiologist looking for on a mammogram?
When reading a mammogram, a radiologist is looking for the presence of a new mass, a grouping of calcifications, an asymmetry, architectural distortion, skin thickening, nipple changes, lymph node enlargement, and more. The radiologist will compare your most recent mammogram with your prior mammograms to detect any changes. Each of these descriptors can be benign (non-cancerous) or malignant (cancerous). As a result, if any of them appears on your mammogram, you may get called back for extra mammogram views and possibly an ultrasound.
If you’re called back, please don’t worry until we tell you to worry. Most patients who are brought back for additional views and/or an ultrasound do not have cancer.
Read Dr. Emily Stone’s blog post, “Screening Mammograms: When To Start, Odds Of Getting “Called Back,” And How They Can Save Your Life”>
How should women best prepare for a mammogram?
It’s best to be as relaxed as possible and not wear deodorant the day of your mammogram. If possible, make sure your provider has access to your prior mammograms. Learn more about how to prepare for your screening mammogram at VPFW.
Why can’t you wear deodorant to a mammogram?
Deodorants and antiperspirants have tiny aluminum particles that help prevent sweat from coming to the surface of the skin. These tiny particles can affect how accurately your mammogram can be read by a radiologist. On a mammogram, the particles show up as tiny white dots that can look like calcifications. There are many different causes for calcifications, most of which are benign; but sometimes calcifications can be an early sign of breast cancer. If these white dots appear on your mammogram, your radiologist will likely order more tests to determine their source.
What is a 3D mammogram?
A 3D mammogram is the acquisition of images of the breast tissue in 1mm thick slices, allowing the radiologist to separate out normal breast tissue from potential cancers. The positioning for the images is the same as in a 2D mammogram, but the acquired images in a 3D mammogram show us more detailed information.
Are there certain people who need a 3D mammogram?
Everybody should get a 3D mammogram. This is the best screening mammogram study offered to all women. Most insurance companies cover 3D mammograms.
When is a breast ultrasound necessary?
A breast ultrasound is usually used as a diagnostic tool when a patient feels a “lump” or has a new finding on or in her breast. It can also be used as a supplemental screening tool; however, it has limitations.
When is a breast MRI necessary?
A breast MRI is the most sensitive tool for the detection of breast cancer. There are two main types of breast MRIs:
- Regular breast MRI – to be done in patients with a new cancer diagnosis, silicone implant integrity assessment, or as a screening tool for patients with increased risk of developing breast cancer.
- Fast (aka abbreviated) breast MRI – to be done in women who desire supplemental imaging with a breast MRI. Anyone can have a fast MRI; however, it is highly recommended in any woman with dense breast tissue. Insurance companies do not get billed. The patient pays out of pocket $350.
Patients with known genetic mutations or radiation therapy to the chest between the ages of 10 and 30, as well as in a few other instances, should have annual screening MRIs in addition to annual screening mammograms. Women diagnosed with breast cancer at 50 or younger OR who show dense tissue on mammograms should also have annual breast MRIs.
Is there anything women with dense breasts should know about mammograms and breast health?
Yes! Your mammogram results will show if you have dense breast tissue. If this is the case for you, here’s what to know:
- It’s difficult to read your mammograms. Dense tissue is white, and so is breast cancer. Please advocate for supplemental screening with a breast MRI (fast breast MRI if you have no increased risk due to family history, or regular breast MRI if you’re at increased risk).
- If you aren’t doing monthly breast self-exams, start now. If you’re still menstruating, do your breast self-exam 10 days after the start of your menstrual period. This is the point in your cycle when your breasts are least likely to be tender or swollen. Otherwise, pick the 1st of every month to do your exam. You’re looking to determine what normal lumps and bumps exist in your breasts so that if a new one should form, you’ll know.
- Cancer grows in glandular tissue. The increased glandular tissue in dense breasts increases your risk of developing breast cancer.
When is a screening mammogram necessary before age 40?
If a patient has a parent or sibling who has been diagnosed with breast cancer before age 50, the patient should begin annual screening mammograms earlier than the recommendation for average-risk women, which is age 40. A screening mammogram should be done 10 years prior to the diagnosis of a first degree relative. For example, if a patient’s mother was diagnosed with breast cancer at the age of 41, the patient’s annual screening mammograms should begin at age 31.
At what age should women stop getting mammograms?
There isn’t an upper age limit for screening mammograms. Screenings should be done every year beginning at the age of 40 until the woman is within 10 years of her possible death (determined by factors such as severe heart disease, an untreatable cancer diagnosis, etc.).
Should men be getting screening mammograms?
Men have a 1 in 1,000 risk of developing breast cancer. They should be aware of any changes in their breast tissue; however, screening mammograms typically aren’t necessary. Men with certain genetic mutations might get occasional mammograms as recommended by their primary care doctor or cancer doctor.
Any last advice?
Get your screening mammograms EVERY year. DO NOT SKIP A YEAR, no matter how busy life gets. And if you feel anything different in your breasts, see your doctor immediately.
Learn more about mammograms at VPFW or schedule a mammogram at one of four VPFW locations (West Creek, St. Francis, Prince George, or Koger Center), call VPFW at 804-897-2100 or message us to schedule online.