From detection to symptoms to risk factors, Melissa Foster, N.P., discusses how female reproductive cancers differ and what you can do to reduce your risk.
For each type of gynecologic cancer, early detection and timely treatment are important for improving outcomes. But the 5 main cancers of the female reproductive system (vulvar, vaginal, cervical, uterine, and ovarian) do not share the same symptoms, treatment options, methods for detection, or even risk factors. That’s because each portion of the female reproductive system is made up of different types of cells – meaning each part is affected by cancer differently. This is one of the many reasons gynecologic cancer diagnoses can be complicated and confusing.
To gain a better understanding of the differences in these 5 gynecologic cancers, let’s follow the order in which your provider will typically conduct your pelvic exam. We’ll cover each part of the female reproductive system and how cancer presents in each, as well as what you can do to reduce your risk and/or improve outcomes.
Vulvar Cancer
Once you have scooted all the way down to the edge of the bed, your provider will examine your external genitalia, also known as the vulva. This includes the inner and outer lips, the clitoris, the opening of the vagina and the glands found there. Vulvar cancer is rare. It’s reported to affect approximately 5,000 women in the U.S. each year. That means approximately 1 in 333 women have a chance of developing vulvar cancer during their lifetime.
During this portion of your exam, your provider will be looking for areas of color change, lumps, bumps, and other irregular findings that you may not have noticed. It is likely, with regular exams, to find vulvar cancer early, in the pre-cancerous phase or stage 1 phase.
Symptoms of Vulvar Cancer
Symptoms of vulvar cancer may include:
- Itching that will not go away
- Skin that appears lighter or darker than usual; it can be red or pink
- A bump or lump, which could be red, pink or white, and could have a wart-like or raw surface
- Pain or burning
- Bleeding or discharge not related to the normal menstrual period
- Open sore (especially if it lasts for a month or more)
- Cauliflower-like growths similar to genital warts
- Ulcer in the genital area
Diagnosis and Treatment of Vulvar Cancer
Typically, if an area of concern is found during examination of your vulva, your provider may ask you to return for a biopsy that can be done in the office with local anesthesia (numbing medication given by injection). Generally, vulvar cancer can be treated with a simple surgery that may be performed by your general gynecologist or a gynecologist oncologist.
Vaginal Cancer
Once your vulva has been assessed, your provider will assess your vagina, also known as the “birth canal.” The walls of your vagina are susceptible to cancerous changes, but this is the most rare of the gynecologic cancers. About one in every 1,100 women in the U.S. will be diagnosed with vaginal cancer Typically women ages 50-70 are the most affected.
Symptoms of Vaginal Cancer
Precancerous and early stages of vaginal cancer usually have NO symptoms! Just another reason to continue to have those annual pelvic exams. More advanced stages of vaginal cancers may exhibit some of the following symptoms:
- Unusual vaginal bleeding
- Pain
- Problems with urination or bowel movements
- Watery vaginal discharge
- Lump or mass in the vagina
Diagnosis and Treatment of Vaginal Cancer
If your provider detects anything abnormal during examination of your vagina, they may conduct a colposcopy. A colposcope is a lighted magnifying tool that your provider can use to more carefully inspect the surface of your vagina for abnormal cells. They may also conduct a biopsy, removing a sample of suspicious tissue to be sent to a lab to test for cancer. Both of these procedures can usually be done in the exam room.
If vaginal cancer is detected, you’ll be referred to a gynecologic oncologist who may conduct more exams and testing to determine whether the cancer has spread and what stage it is in. Most vaginal cancers can be cured with surgery or radiation therapy.
Cervical Cancer
Once your provider has fully assessed your vulva and vagina, the focus is now directed to the cervix. This is the “neck” of the uterus that dilates to allow a baby to move from the womb through the birth canal. This is where we conduct a Pap test to screen for cervical cancer. Approximately 0.7 percent of women will be diagnosed with cervical cancer at some point during their lifetime, based on 2017–2019 data.
Symptoms of Cervical Cancer
Similar to vaginal cancers, precancerous and early stages of cervical cancer most often do not have symptoms. However, more advanced stages may demonstrate the following symptoms:
- Vaginal discharge
- Abnormal vaginal bleeding
- Vaginal odor
- Pain
Screening of Cervical Cancer
Cervical cancer is the only gynecologic cancer that can be PREVENTED through routine screening. This screening is called a Pap test, which can be conducted during your routine pelvic exam. During a Pap test, your provider will collect and examine cells from your cervix to look for abnormal cells that can lead to cancer.
The Pap test used to be performed every year by all providers, but through many years of research, it was determined that it may be unnecessary to collect cervical cells every year. Depending on the testing, some providers go as many as 5 years between performing a Pap test. Talk to your doctor to see what they recommend based on your health history.
Fun Fact: Dr. Papanicolaou, originally of Greece, did all the testing to formulate the Pap test that has saved many women from cervical cancer. But that’s not the fun part! His wife, Mrs. Papanicolaou really deserves the gold medal because she allowed her husband to collect cells from her own cervix DAILY for 21 YEARS to help!
Diagnosis and Treatment of Cervical Cancer
If the results of your Pap test reveal any abnormalities, you will be asked to visit your provider again so that a colposcopy can be performed. Your provider will use a large microscope to look at your cervix more closely and possibly take biopsies to be analyzed in a lab.
Follow up from a colposcopy is dependent on its results. Precancerous diagnoses will likely be followed by your general gynecologist conducting outpatient procedures to treat or remove the precancerous cells.
If there is a cancer diagnosis, you will be referred to a gynecologic oncologist. Treatment is dependent on the stage of the cancer.
Uterine Cancer
After the Pap test is complete, your provider will likely move on to the bimanual exam – the portion of the pelvic exam where two hands are used to check internal pelvic organs. One to two fingers are inserted inside the vagina, and the other hand feels like it’s kneading your abdomen. During this exam, the provider is usually first assessing your cervix and uterus as a whole. The uterus is also known as the “womb” and is the organ where a baby will develop during pregnancy. The size and shape of your uterus is assessed as best as possible based on your anatomy. If there is any question or concern about the uterine shape, size, or quality of pain (i.e. sharp, dull, stabbing, burning, throbbing) during the exam, a transvaginal ultrasound may be ordered.
There is no screening test for uterine (also called endometrial) cancer. The endometrium is the lining of the uterus – where the period comes from if you are still having them. This area can develop cancer, especially in postmenopausal women who no longer have periods. In the U.S., approximately 2.8% of women will be diagnosed with uterine cancer in their lifetime. Women of any age who are obese have an increased risk of endometrial cancer compared to women with a normal weight.
Symptoms of Uterine Cancer
The first sign of uterine cancer is usually bleeding after menopause or irregular bleeding in women before menopause. If you notice changes to your menstrual cycles, especially consistently heavier bleeding and/or irregularity between cycles, mention it to your provider to determine if any additional follow up is warranted.
Diagnosis and Treatment of Uterine Cancer
I always recommend my patients think of bleeding after menopause like finding a lump in their breast – we will do a workup for cancer, but most of the time we do not find anything wrong. The workup includes an endometrial biopsy performed in the office and a transvaginal ultrasound. Some providers may do the biopsy before the ultrasound while others may wait to see the results of the ultrasound.
Most endometrial cancers are found in the early stages and are cured with a hysterectomy.
Ovarian Cancer
During the bimanual exam, your provider will also move to either side of your uterus to attempt to assess your ovaries (the organs that release eggs during childbearing years). If there is a mass or unusual pain noticed on either side, you will likely be scheduled for a transvaginal ultrasound to better view your ovaries and the area around them.
Approximately 1.1 percent of women will be diagnosed with ovarian cancer at some point during their lifetime. The term “ovarian cancer” is often used to describe cancers that begin in the cells in the ovary, fallopian tube, or peritoneum (tissue that lines the abdomen and most of the organs in the abdomen). These cancers are closely related and are treated the same way.
Symptoms of Ovarian Cancer
Unfortunately, the symptoms of ovarian cancer are vague, often leading to misdiagnosis. Ovarian cancer used to be called the “silent killer” because it seemed that symptoms did not develop before the cancer had advanced so much that the chance of curing it was unlikely. However, according to the Foundation for Women’s Cancers, “recent studies have shown this term is untrue and that the following signs are much more likely to occur in women with ovarian cancer than in women in the general population – even in patients with early-stage disease.”
- Bloating
- Pelvic or abdominal pain
- Difficulty eating or feeling full quickly
- Urinary symptoms including urgency or frequency
Women with ovarian cancer report that symptoms are persistent and represent a change from normal for their bodies. If you are experiencing these symptoms almost daily for more than a few weeks, you should visit your gynecologist.
Other symptoms have been commonly reported by women with ovarian cancer such as fatigue, indigestion, back pain, pain with intercourse, constipation, and menstrual irregularities. These symptoms are not as useful in identifying ovarian cancer because they are also found in equal frequency in women in the general population who do not have ovarian cancer.
Diagnosis and Treatment for Ovarian Cancer
Diagnosis of ovarian cancer takes into account the frequency and number of ovarian cancer symptoms listed above. If symptoms present a concern about ovarian cancer, the first step is to have a transvaginal ultrasound to determine if there is a visible mass in or around your ovaries.
If an abnormality is discovered during your ultrasound, your provider may order blood work to help determine the type of ovarian cancer. These labs are NOT used as screening tools because noncancerous factors can also elevate them and cause unnecessary anxiety. If there is a further concern for ovarian cancer, you will be referred to a gynecologic oncologist who will determine treatment planning.
What’s Next: Assessing Your Risk Factors
At this point your physical pelvic exam is complete. We will assume your exam has been normal. If your provider hasn’t already, you may discuss your risk factors for different cancers. Please note: each provider does this differently. It may be done before or during the physical exam. Or, if you’ve been seeing them for a long time, they may know your risks very well and may not discuss them in as much detail mentioned here.
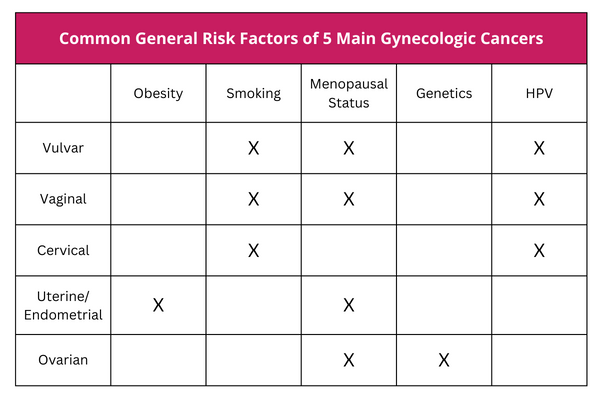
Here are some common general risk factors for each type of female reproductive cancer:
HPV – The Human Papillomavirus
Exposure to HPV (the human papillomavirus) can increase your risk of vulvar, vaginal, and cervical cancers.
The good news is, there is now a vaccine that can help prevent these cancers as well as other infections caused by HPV. In 2018, the FDA approved the Gardasil series for women (and men!) ages 27-45 after it had previously only been available to people ages 9-26. It is recommended for women to receive this series of vaccinations.
According to the study submitted for FDA consideration, for approximately 3,200 women age 27 through 45, followed for an average of 3.5 years, Gardasil was 88 percent effective in the prevention of a persistent infection, genital warts, vulvar and vaginal precancerous lesions, cervical precancerous lesions, and cervical cancer related to the strains of HPV covered by the vaccine.
Learn more about HPV and the HPV vaccine in Dr. Mark Hyde’s blog post, What Your Family Needs to Know About HPV and The HPV Vaccine and Dr. Kristen Lawson’s blog post, FAQ’s About HPV and The HPV Vaccine as New Mandate Takes Effect.
Obesity
Obesity is a risk factor for many medical problems. In terms of affecting your risk for gynecologic cancers, obesity is most concerning for uterine/endometrial cancer. Obesity can also make diagnosis of uterine and ovarian cancers difficult due to limitations during the pelvic exam that can result in difficulty feeling abnormalities.
Menopausal Status
Most gynecologic cancers are more prevalent after menopause, EXCEPT for cervical cancer. Cervical cancer is most prevalent in women ages 30-50.
Genetics
Ovarian cancer is the type of female cancer that carries the most genetic risk, but genetics can be a factor in some endometrial/uterine cancers. Family history of breast cancer (especially a history of MALE breast cancer), colon cancer, and endometrial cancers should be discussed with your provider. You may need to see a genetic counselor to determine specific recommendations.
Other Risk Factors:
Beyond these more general risk factors, some gynecologic cancers come with their own individual risk factors. Take note of these and discuss with your provider if they are relevant to you.
Ovarian Cancer: Infertility, Ashkenazi Jewish heritage
Endometrial/Uterine Cancer: Taking estrogen without progesterone for menopause hormone therapy, not reaching menopause until after age 52, diabetes, hypertension, never being pregnant, use of tamoxifen (after breast cancer treatment)
Vaginal Cancer: Use of or exposure to Diethylstilbestrol (DES)—a hormonal medicine used many years ago during pregnancy to prevent miscarriage
Vulvar Cancer: Lichen sclerosis—a chronic skin condition that causes thin, white patches of skin, usually in the genital area
Give Yourself Your Best Chance Against Cancer
Once your exam is complete, you will be up to date with your gynecologic cancer screening for another year. We recommend maintaining your routine pelvic exams and being open about your family history and personal risk factors – so that together, you and your provider can give you the best chance against cancer.
Between exams, listen to your body and let your provider know if you notice abnormal changes or symptoms, especially if they persist for more than a few weeks. There are many non-cancerous conditions that could be the cause, but if it is cancer, promptly bringing up your symptoms will help your doctor diagnose it earlier, when there’s a better chance for effective treatment.
If you’re not sure if you should come in, call us at 804-897-2100 and press 2 to speak to one of our phone advice nurses. They are great at helping you work through whether you can wait or need to be seen soon!
To make an appointment with an OB/GYN provider at one of our Richmond, VA, locations, call VPFW at 804-897-2100 or message us to schedule online.
