Dr. Amy Demarchi explores how the latest research findings have led to new do’s and don’ts for treatment and prevention of this common breastfeeding affliction.
Summary: Mastitis is a painful inflammation of the breast that commonly affects breastfeeding women, especially in the early weeks. New research from the Academy of Breastfeeding Medicine shows that mastitis encompasses a spectrum of conditions and that treatment should focus on decreasing inflammation and tempering stimulation – reversing some past guidelines. We explore how to recognize the symptoms, treat them effectively, and prevent future occurrences.
- What is mastitis? Mastitis includes a spectrum of conditions marked by inflammation in the breast.
- What causes mastitis? Narrowed milk ducts, unresolved hyperlactation, tissue trauma, a disruption of the milk microbiome
- What does mastitis look like? Redness, swelling, pain, fatigue, and/or flu-like symptoms.
- Mastitis treatment: Apply ice or cold compress, use ibuprofen or acetaminophen, use sunflower or soy lecithin, feed at the breast on baby’s cues (but stop if no milk is flowing), and consult your provider. Antibiotics may not be needed in most cases.
- Outdated treatments to avoid: Applying deep massage or squeezing the breast, increasing milk removal and trying to “empty the breast,” applying heat
- How to prevent mastitis: Feed at the breast or hand express only in response to baby’s cues, avoid pumping large amounts of milk to store, and seek lactation support for hyperlactation (oversupply).
Breastfeeding is a powerful way to nourish and bond with your baby. However, new parents should understand that it can sometimes come with unexpected complications that can impact your breastfeeding goals.
One of the most common – as well as painful and frustrating – issues nursing mothers may face is mastitis. What is mastitis, and what causes it?
We’ll explain what mastitis looks like and explore the Academy of Breastfeeding Medicine’s revised protocol for treatment and prevention based on new clinical research. Continue reading to find evidence-based answers and relief from the team at Virginia Physicians for Women.
What Is Mastitis?
Mastitis is an inflammation of the mammary gland that often occurs in breastfeeding women. According to the Academy of Breastfeeding Medicine (AMB) Clinical Protocol #36: The Mastitis Spectrum, Revised 2022, mastitis is no longer considered a single issue but a spectrum of conditions resulting from inflammation of the milk ducts and swelling due to fluid buildup in the breast’s supportive tissue.
The revised ABM protocol includes the following conditions in the spectrum of mastitis:
- ductal narrowing (often referred to as “plugged ducts”)
- inflammatory mastitis
- bacterial mastitis
- phlegmon
- abscess
- galactocele
- subacute mastitis
The underlying concern of all of these conditions is inflammation.
While early postpartum engorgement is not included in the spectrum of mastitis conditions, it can have similar symptoms and is covered in the ABM’s revised guidelines. If engorgement is managed appropriately, it should not progress to conditions on the mastitis spectrum.
While mastitis can happen at any time during lactation, it’s most common during the first few weeks of breastfeeding. This is a time when both mother and baby are adjusting to the breastfeeding process and the mother’s milk production is regulating.
What Causes Mastitis?
Several factors can contribute to breast inflammation and cause mastitis in breastfeeding women, including:
- Narrowed or blocked milk ducts (often referred to as “plugged ducts”)
- Unresolved hyperlactation (an oversupply of milk), often due to overstimulation of milk production
- Tissue trauma, which can result from aggressive massage
- Mammary dysbiosis (disruption of the milk microbiome)
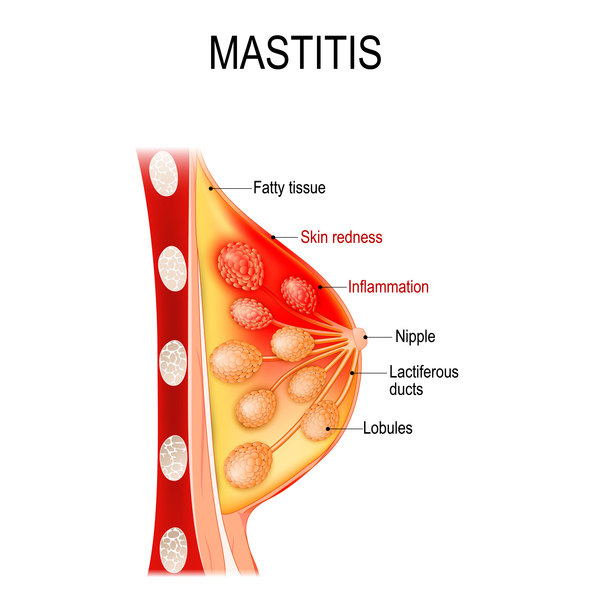
Milk is stored in groups of milk sacs called lobules. It flows through a series of tubes in the breast called ducts.
When the body produces more milk than the baby drinks, pressure develops in the breast. The oversupply of milk is often the result of going longer stretches between feedings, such as when the baby begins sleeping through the night or if the baby is not feeling well and nurses less. Or, it could be due to hyperlactation (an oversupply of milk), which can be caused by overstimulation of milk production.
The body will sometimes respond to the stress of pressure building up from an oversupply by becoming inflamed. The inflammation can constrict the milk ducts and cause a blockage. There is not actually a “plug” of milk causing a blockage. However, the narrowing of the ducts due to the swelling results in the milk flowing more slowly.
Aggressive massage can cause tissue trauma. This can lead to an abscess or other conditions on the mastitis spectrum.
Mammary dysbiosis is a disruption of the breast’s microbiome that can lead to bacterial mastitis. Hyperlactation, or breast milk “oversupply,” and excessive pumping can facilitate dysbiosis.
What Does Mastitis Look Like?
Typical signs of mastitis include a range symptoms that can look or feel like:
- A red or discolored, swollen area on the breast that may feel warm or tender to the touch.
- A hard lump or wedge-shaped area on the breast.
- Pain or a burning sensation during nursing.
- Flu-like symptoms such as fever, chills, and body aches. (These symptoms may occur with or without infection.)
- Fatigue or feeling generally unwell.
Mastitis Treatment: What to Do When You’re in Pain
Prompt treatment of mastitis symptoms can halt its progression in the spectrum of conditions and prevent the need for antibiotics. However, traditional treatments such as deep massage and increased breastfeeding or pumping will likely make symptoms worse. These outdated treatments can result in more inflammation and more milk production, leading you further down the spectrum of mastitis conditions.
Instead, we recommend these evidence-based treatment options that focus on reducing inflammation:
- Apply ice or a cold compress to decrease swelling (as you would for a sprained ankle)
- Take ibuprofen or acetaminophen to reduce inflammation and provide pain relief
- Take sunflower or soy lecithin (5–10g daily by mouth) to reduce inflammation in ducts and emulsify milk.
- Gentle lymphatic massage may help reduce swelling.
- “Hands-on pumping” and hand expression are okay, but avoid excessive manual force
- Maintain a normal feeding or pumping schedule rather than always starting with the afflicted side.
- Stop feeding or pumping if no milk is flowing.
- Antibiotics are not usually needed, but may be necessary for bacterial mastitis.
If symptoms worsen or persist for more than 24 hours, contact your doctor at Virginia Physicians for Women. While these general recommendations apply to all conditions on the mastitis spectrum, you should ask your doctor for condition-specific interventions.
Be mindful of outdated treatments that are no longer recommended but are still circulating in many online resources.
- Avoid deep massage and massaging devices that can damage tissue, potentially leading to an abscess
- Don’t increase the quantity or frequency of pumping or feeding on the afflicted side. It will stimulate an excessive milk supply and continue the cycle of mastitis.
- Avoid applying heat, which can provide some comfort but worsens symptoms.
Can you breastfeed if you have mastitis?
As long as the milk is flowing, it is safe for breastfeeding women to continue to breastfeed. However, you should not increase your frequency or amount of breastfeeding on the afflicted side in an attempt to “empty the breast.” Do not continue breastfeeding or pumping if no milk is flowing. The swelling must be reduced first.
Mastitis is not contagious and does not pose a threat to the breastfeeding baby. Breastfeeding and breast milk are safe with mastitis, abscesses, and taking antibiotics.
How to Prevent Mastitis
Preventing mastitis starts with good breastfeeding habits and support.
- Know that it is normal for lactating breasts to feel full, lumpy, and even painful due to full milk sacs. Likewise, be reassured that pain and redness you may experience, especially after a longer stretch without feeding, is most likely due to inflammation rather than infection.
- Resist any temptation to massage out a “plug.” There is no such thing as a milk plug, and this action will only cause more inflammation, pain, and possibly tissue damage.
- If you are pumping, mimic the frequency and volume of milk that you would be breastfeeding your baby. Avoid pumping large amounts to build up a freezer stash.
- Wear a comfortable and supportive bra.
- If you are experiencing hyperlactation (consistent oversupply of milk), seek support from a lactation consultant to reduce your milk production.
Need Support with Breastfeeding or Mastitis?
If you have concerns about mastitis, please don’t hesitate to call our office at 804-897-2100 and speak with our medical advice line.
Breastfeeding can be a difficult journey with many questions. Don’t ever feel ashamed to ask for lactation support if you need help. The proper support can ensure you and your baby stay healthy. You can also find more breastfeeding resources in Dr. Hartle’s Formula, Breastfeeding, and Mental Health Resources for Richmond Area Moms blog post.
VPFW’s caring OB/GYN providers in Richmond, VA are here to help you navigate every stage of motherhood. We offer support from pregnancy to postpartum recovery and beyond. Schedule an appointment for your health today!
